
Dual Diagnosis: Understanding Co-Occurring Disorders, Treatment Overview & More
Mental health disorders and substance use disorders (SUD) often go hand in hand. For many who have struggled with mental illness, they may feel as…
We’re Here to Help 720.891.4657

Mental health disorders and substance use disorders (SUD) often go hand in hand. For many who have struggled with mental illness, they may feel as…

Schizophrenia is a severe mental health condition that can influence a person’s thought processes, feelings, and behaviors. It can dramatically affect a person’s daily life…

More than 40 percent of people report having trouble sleeping because they’re worrying about work, according to Forbes Magazine. The truth is, many of us…

“Walk a mile in someone else’s shoes.” There’s maybe no better example of something being easier said than done – especially when it comes to…

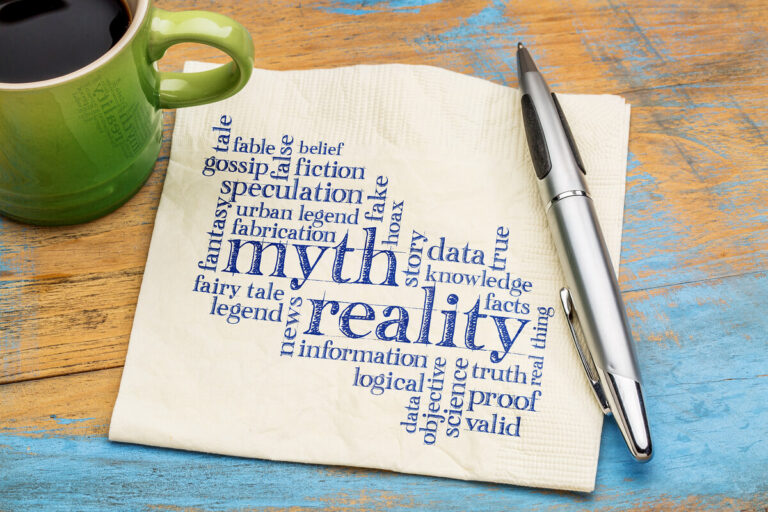
You’ll hear all kinds of promises when looking around at various treatment centers. While some of them may be true, it’s also important to…

According to a recent survey, 10 percent of adults in the United States will struggle with a drug or alcohol addiction in their lifetime. That…

You’ve decided to get help—and that’s great. But it’s also important to make sure that you’re receiving the kind of care that can help you…

Whether you’re struggling with a drug or alcohol addiction, finding the right treatment center and program can often feel overwhelming when you’re getting started. Here,…

Your addiction treatment team is focused on empowering your recovery and collaborating with you to meet your needs. You trust that these individuals are experienced,…

Understanding Relapse What Is Relapse? Relapse is when someone who is in recovery from a particular addiction returns to that substance or behavior. Most commonly,…

Understanding Addiction What Is the Definition of Drug and Alcohol Addiction? When someone is struggling with a drug or alcohol addiction, they experience a compulsive…

Imagine a spectrum. On one end is your Aunt Helen. She drinks half a glass of white zinfandel on Thanksgiving and you can tell she’s…

Heroin and prescription opioids like OxyContin® are familiar sounding drugs to most people. In recent months, the opioid epidemic in America has been well reported…

There are many possible triggers for relapse. People, places, and things associated with drinking and drug use are major triggers. Stress is another major trigger….

You probably started out taking painkillers for a legitimate reason—pain following a procedure or operation. You weren’t aware how powerful the drugs are or how…

OxyContin (Oxycodone) is a drug that is used to relieve severe pain that may occur in patients with serious physical trauma cancer or other debilitating…

Recovery here means access to evidence-based therapies, personalized treatment plans, and a supportive community—all in a setting that promotes physical, emotional, and mental healing. If…

When your loved one was living with addiction, drugs or alcohol were the most important thing. After rehab, that changed—but maybe not in the…

There are so many emotions at a time like this. On one hand, you’re so relieved that your loved one is in treatment for drug…

After a child, family member or close friend completes a professional addiction treatment program, you can play an important role in decreasing the chances of…

If the COVID-19 pandemic has taught us anything, it’s that being home alone five days a week can get to you. If you’re able to…

Depending on how you look at it, New York City can be either the best or the worst place to launch a new life after…

Addiction taught you the importance of building a healthy support network of loved ones and friends. You also learned valuable relapse prevention techniques like socialization…

Do you drink too much? “Yeah, probably,” you think to yourself. But when the coronavirus (COVID-19) has you isolated from your friends and family and…

Life is full of steppingstones – both big and small – to get you to where you want to go. For example, an internship is…

By the time I got to The Raleigh House, my parents were well aware of the damage their enabling and inability to set firm boundaries…

Healing is more than just physical recovery—it’s about achieving whole-body wellness and emotional balance. At The Raleigh House’s Center for Integrative Behavioral Health in Denver,…

In our last two blog posts, we explained how family education and emotional support can help a loved one recover from drug addiction. Today, we’ll talk…

Rehab is one of the most intense experiences you’ll ever have in your life. Name an emotion and you’ll probably have it during your…

You’ve made the decision—and taken the action required—to rebuild your life. And when you return from rehab, you may expect everything to be different….

Once you’ve made the decision to enter rehab, it seems like everything should simply fall into place. Unfortunately, it doesn’t always work out that way….

When you’re in the sinkhole of addiction, it can be impossible to imagine ever feeling happy or good again. But it is possible, especially when…

Once you’ve made the decision to get your life back on track, there is still one very important decision left to be made—which rehab…

Psychological trauma is what happens when the amount of stress one faces overwhelms their ability to cope. It can be caused by many things, including…
The peace lily is a vibrant plant that can make any space instantly more inviting. The white blooms of a peace lily are a wonder…

How to Prevent Relapse: Managing Your Emotions Relapse may not be you think it is. It’s a gradual process that can actually begin weeks or…

“You never really understand another person until you consider things from his point of view—until you climb inside of his skin and walk around in…

We all know by now that drugs and alcohol can affect your pregnancy, but prescription painkillers can be just as harmful. Taking prescription painkillers while…

Your loved one has been through a lot before they made the decision to seek addiction treatment. While you’re proud that they are moving their…

You didn’t expect rehab to be easy. In fact, you came ready for a fight. It was that mental toughness and determination that got you…

Expectations are high this time of year. You’ve got to buy and wrap presents, string lights, put up the tree, bake cookies, travel or host…

Heroin has left your life in shambles and—yet—you’re so scared to let it go. It actually makes perfect sense. Heroin has taken away your self-worth,…
If you started taking painkillers to treat chronic pain, you may be asking yourself how you can live without them. The truth is that painkillers…
When an older adult is clearly drinking too much or abusing drugs, we tend to have one of two responses: But both of those…

Outpatient rehab sounds great. You can tackle your addiction head-on, while still making money and living in the comfort of your own home. And while…

One of the reasons that addiction is so difficult to overcome is that drugs impact the way your brain works. They create chemical imbalances that…

“I can take painkillers or I can live in pain.” This is likely a message you’ve heard before if you have a loved one who…

Anyone who drinks and is concerned about their health likely knows the recommended U.S. safe drinking limit—two drinks a day for men and one…

My life before the Raleigh House was a mess. I started drinking heavily at 18. Then I got into cocaine meth and any pill that…
Did you know that more people use prescription opioids than tobacco products? It’s true. In fact, there are more people with substance abuse disorders than…
"*" indicates required fields